Background: Venous thromboembolism (VTE) is the second most common contributor to harm in hospitalized pediatric patients.The presence of a central venous catheter (CVC) remains the most potent risk factor for the development of VTE in children. Children with chronic illnesses often require multiple CVCs throughout their lifetime. There is limited evidence regarding either risk factors for recurrent VTE with subsequent CVC placement or efficacy of secondary prophylaxis.
Methods: We performed a single center retrospective cohort study and included subjects from 0-18 years of age with an initial CVC-associated VTE (CVC-VTE) that occurred between 1-1-2003 to 12-31-2013. Subject data was collected from the initial CVC-VTE event until either the end of the study period (9-30-2014) or a recurrent VTE event. Data collection included demographics, CVC details (total number of CVCs placed during the study period, line type, and duration), underlying medical conditions (acute and chronic), thrombophilia, and anticoagulation regimens. During the study period, our clinical practice included secondary VTE prophylaxis with enoxaparin for subsequent CVCs as long as a contraindication to anticoagulation did not exist. The enoxaparin dosing for prophylaxis dosing varied throughout the study period. The association between CVC-VTE recurrence and VTE risk factors for the first subsequent CVC was assessed using logistic regression. A forward stepwise selection approach was used for model building. Variables with a p-value < 0.15 on univariate analysis were included in model building as well as variables deemed clinically significant.
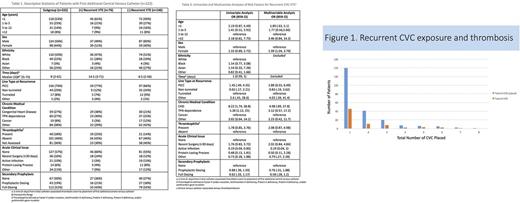
Results: During the study period, 432 subjects had an initial CVC-associated VTE with a mean follow-up time of 27.3 ± 29.6 months. 222 (51.4%) had 1 or more additional CVCs placed with a mean of 1.8 ± 1.3 CVC per subject (Figure 1). For the entire cohort, 111/432 (25.7%) had a recurrent CVC-VTE. Limiting the analysis to the first additional CVC placement, 76/222 (34%) patients had a recurrent CVC-VTE. 67/222 (30%) of patients did not receive secondary prophylaxis. Demographics and distribution of VTE risk factors are listed in Table 1. On univariate analyses, congenital heart disease (OR 8.22; 95% CI 1.74, 38.8) and TPN dependence (OR 5.28; 95%CI 1.12, 25) were associated with an increased risk for VTE recurrence with the first additional CVC placement (Table 2). On multivariable analysis, none of the VTE risk factors remained statistically significant (Table 2).
Conclusions: Over half (222/432) of all children with CVC-VTE in our study required a subsequent CVC. In those who had a subsequent CVC, 50% (111/222) experienced a recurrent CVC-VTE. This is an extremely high risk of thrombosis in a heterogeneous group of children with chronic medical conditions. On multivariable analysis we were unable to identify additional risk factors for VTE recurrence. While the use of secondary prophylaxis either prophylactic (0.76, 95%CI 0.31-1.88) or full dose (0.58, 95%CI 0.28-1.2) had associated odds ratios consistent with a decrease in VTE recurrence, they did not meet statistical significance. A history of a prior CVC-VTE is likely the strongest risk factor for recurrent CVC-VTE. This very high risk group (patients with prior CVC-VTE who require a subsequent CVC) is an ideal population to target in future interventional studies.
Raffini: Green Cross Inc: Consultancy; CSL Behring: Consultancy; Bayer: Consultancy; Genetech: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal